Binge eating disorder in (type 2) diabetes is not only a frequent diagnosis, it’s also the most common eating disorder in the United States.
What is binging (binge eating)??
Binge eating disorder (BED) is defined as frequently (at least once a week for three months or more) consuming large amounts of foods and feeling unable to stop eating. Binge eating episodes are associated with eating rapidly, regardless of hunger, until extreme fullness, and/or associated with depression, shame or guilt.
Many people will have episodes of binge eating/overeating on occasions such as holidays like Thanksgiving or when indulging in a buffet. That does not mean you have binge eating disorder. BED has recurrent episodes with a lack of control to stop eating.
Signs and Symptoms of Binge Eating Disorder
Early detection and diagnosis of all eating disorders is imperative to treatment. Both physical and mental health exams are generally needed for diagnosing binge eating disorder. Some signs and symptoms include:
- Eating rapidly, large amount over a short period of time, or when full
- Feeling out of control around food
- Negative emotions such as guilt, shame, disgust
- Frequent dieting or weight fluctuations
- Eating in secrecy
- Depression and/or anxiety
- Body Dissatisfaction
- Gastrointestinal issues
Most individuals struggling with binge eating disorder will try to hide these types of behaviors. Factors that increase risk of developing binge eating disorder include dieting, psychological issues, family history of eating disorders.
Do people with diabetes binge eat?
Binge eating disorder is common in people with type 2 diabetes. Studies suggest that up to 20% of patients with T2DM have an underlying eating disorder (the most common of which is binge eating) which is much higher than the 2% to 3.5% prevalence seen in the general population.
It is also the most common type of eating disorder in the United States. This includes many women with type 2 diabetes. On average, women develop binge eating disorder in their early to mid-20s. But eating disorders are happening more often in older women. In one study, 13% of American women over 50 had signs of an eating disorder.
The correlation between BED and Type 2 Diabetes is likely from the recommendation from healthcare providers to restrict calories in the form of a diet. We know diets don’t work, and in this care we see more harm than good.
Why do diabetics binge eat?
Dieting drives binge eating patterns. Diets are not sustainable long-term for most people and they promote weight cycling, lead to an increased risk for disordered eating, and create an unhealthy relationship with food.
Since dieting or restricting can lead to binge eating or overeating, many people will feel out of control around food. The Binge Restrict cycle perpetuates this: diet/restrict, feel overly hungry from undereating, binge/overeat, feel shame/guilt, restart diet, and repeat.
Does binge eating raise blood sugar?
Yes, binge eating will raise blood sugars. It can also cause decreased insulin sensitivity, weight gain, and unstable labs. Episodes of binge eating can be more common when blood sugar is low, resulting in over treatment. Instead of a binge, remember to follow the rule of 15 when your blood sugar is low, consume 15g of carbs (4 oz juice/regular pop, 3-4 glucose tablets, 6-7 hard candies, 1 tablespoon sugar) and test again 15 minutes later to confirm blood sugar is rising.
To recover from binge eating in diabetes it’s important to stabilize blood sugars. Drink lots of water, limit high sugar and high salt foods, and get in some movement. Make sure your meals over the next couple days are more protein and fiber based to prevent further blood sugar spikes.
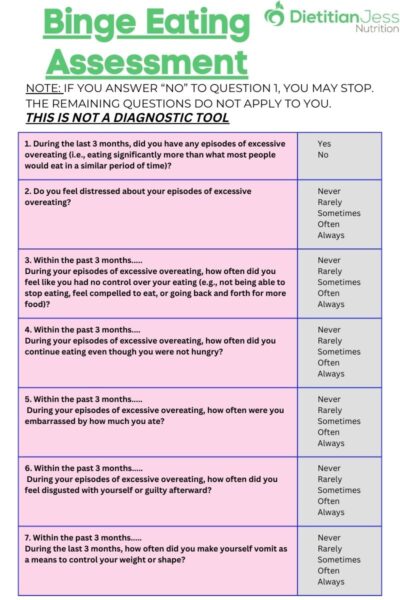
Binge Eating Disorder Test
There is limited published evidence in the assessment and management of binge eating disorder in type 2 diabetes. The first step is for clinicians to screen for binge eating disorder.
The 7-item Binge-Eating Disorder Screener (BEDS-7), is a brief screening tool that can assist healthcare providers in identifying patients who may have BED. Early intervention is associated with better outcomes so being proactive is important.
The questions include asking about eating patterns and behaviors within the last 3 months. NOTE: IF YOU ANSWER “NO” TO QUESTION 1, YOU MAY STOP. THE REMAINING QUESTIONS DO NOT APPLY TO YOU.
- During the last 3 months, did you have any episodes of excessive overeating (i.e., eating significantly more than what most people would eat in a similar period of time)? Yes/No
- Do you feel distressed about your episodes of excessive overeating? Yes/No
Within the past 3 months…
3. During your episodes of excessive overeating, how often did you feel like you had no control over your eating (e.g. not being able to stop eating, feel compelled to eat, or going back for more food)? Never/ Rarely/ Sometimes/ Often/ Always
4. During your episodes of excessive overeating, how often did you continue eating even though you were not hungry? Never/ Rarely/ Sometimes/ Often/ Always
5. During your episodes of excessive overeating, how often were you embarrassed by how much you ate? Never/ Rarely/ Sometimes/ Often/ Always
6. During your episodes of excessive overeating, how often did you feel disgusted with yourself or guilty afterward? Never/ Rarely/ Sometimes/ Often/ Always
7. During the last 3 months, how often did you make yourself vomit as a means to control your weight or shape? Never/ Rarely/ Sometimes/ Often/ Always
NOTE: THIS IS NOT A DIAGNOSTIC TOOL, IT IS A PATIENT REPORTED SCREENING TOOL
How to Recover From Binge Eating Disorder in Type 2 Diabetes
Treating both type 2 diabetes and binge eating disorder is difficult. With BED we want to expose “trigger foods” which typically tend to be that of a less nutritious nature (high carbohydrate, high fat, etc.) Putting too much emphasis on carbohydrates can further trigger disordered eating.
Given that information, it’s important to strive for a balance between the two. Studies of BED therapies focus on pharmacological interventions, psychological and behavioral interventions, or on combinations of two or more approaches.
A meta-analysis completed by the Agency for Healthcare Research and Quality concluded that antidepressant medications, topiramate, lisdexamfetamine, and CBT effectively address major characteristics of binge eating, including increasing abstinence, decreasing the frequency of binge eating, and reducing eating-related obsessions.
Generally there should be a multidisciplinary approach to managing binge eating disorder and diabetes, including a physician, therapist, and dietitian. I have several recommendations coming from the nutrition perspective with an intuitive eating approach.
- Regular access to food
- Assess current nutrition knowledge: which foods contain carbohydrates, which foods affect blood sugar, which foods help balance blood sugars
- Pairing method: pairing carbohydrate with protein, fat or fiber
- Encourage consistent food intake throughout the day
- Evaluate how food makes you feel/how your body responds
Binge Eating Disorder in Diabetes: The Bottom Line:
Binge eating disorder is the most common eating disorder in people with type 2 diabetes but remains underdiagnosed and undertreated. A multidisciplinary, collaborative and holistic approach is required in treatment, including the primary care provider, psychiatrist, therapist, endocrinologist, and dietitian.
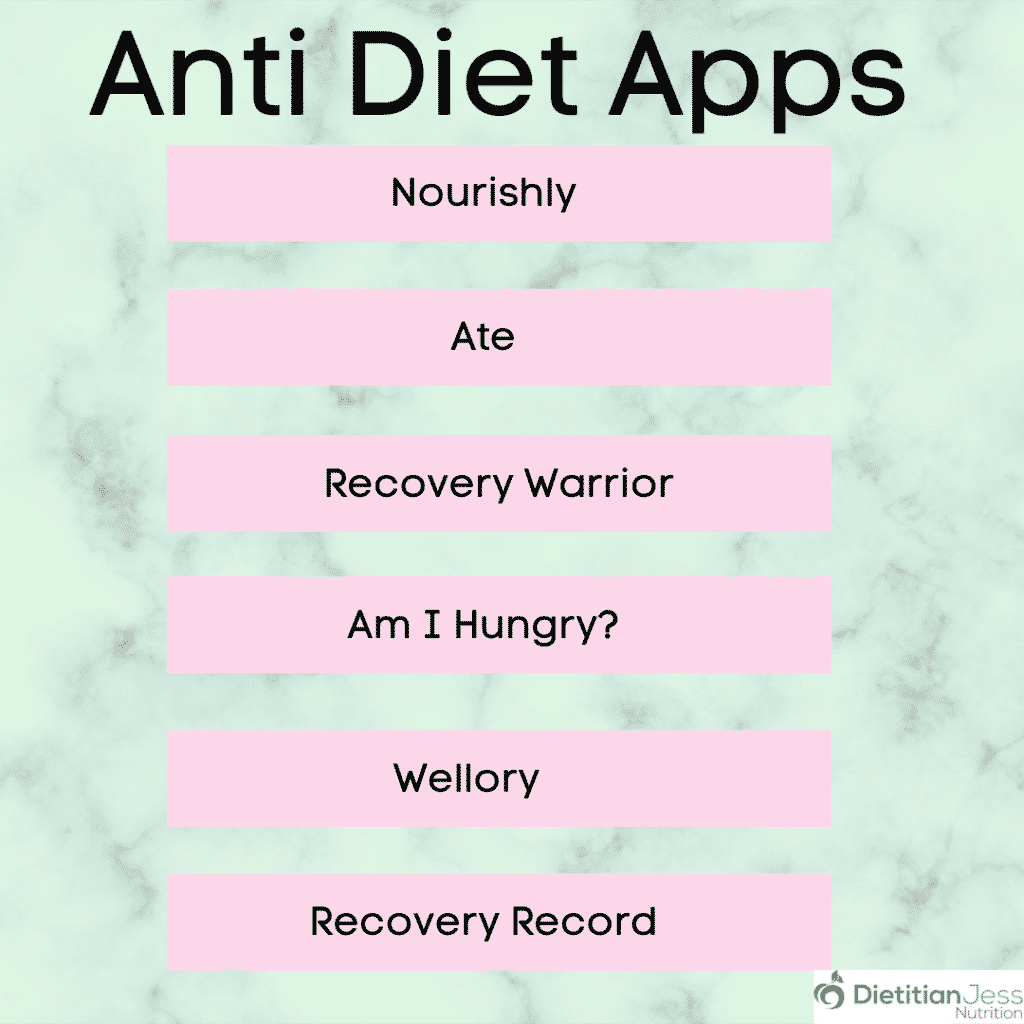
Timely diagnosis is imperative and can help prevent future complications and improve outcomes. If you suspect you are struggling with BED, reach out to your healthcare provider as soon as possible. For more guidance, schedule a consult, or check out a few posts: diet free apps, tips to feel good about your body, and intuitive eating for diabetes for an anti-diet approach to diabetes.